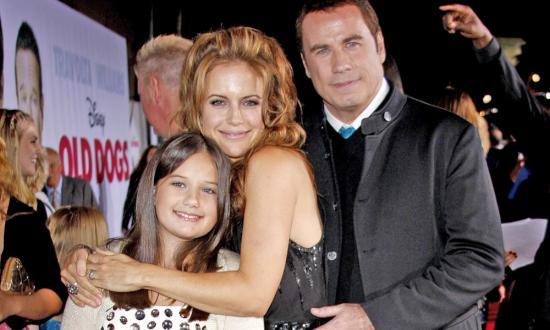
Kelly Preston Dead At 57 From Breast Cancer
The death of Kelly Preston yesterday took all of us – except for those closest to her – by surprise. When a vibrant, beloved soul leaves this world all too soon, we must pause to respect the brevity and ultimate fragility of life. To that end, self-care matters so very much. This is a reminder for us to control whatever we can when it comes to breast cancer. Early detection and maximal risk reduction remain our best defenses against this killer disease that affects 1 in 8 US women (12.5 percent), takes the lives of 1 in 39 US women (3 percent), and will claim approximately 41,760 women and 500 men this year alone.
Only two years passed between Preston’s diagnosis and death. How can this happen, and happen so quickly? The truth is, some breast cancers are more difficult to cure than others, and treatments don’t work in every patient or sometimes work for a while and then stop working. When a woman dies from breast cancer in a short timeframe, this means her cancer was diagnosed at Stage IV (more on that later), and the cancer subtype was likely biologically aggressive, such as “triple negative” or “inflammatory” breast cancers tend to be.
Did Her Pregnancy At Age 48 Play A Role?
For those wondering about Kelly Preston’s pregnancy at age 48 and how that might have contributed to her cancer, note the following facts:
- It is true that those who wait until age thirty-five or older for a first full-term pregnancy carry a 40 percent increase in breast cancer compared to women without kids.[1] The good news, however, is that this elevated risk only lasts for ten to fifteen years and then drops below that of the never-pregnant woman. And anyways, her first full-term pregnancy was at age 30.
- Pregnancy potentially promotes a temporary increase in breast cancer growth, since pregnancy hormones can fuel existing cancer cells (present pre-pregnancy but undetected), but then, these same women enjoy a long-term protective effect since pregnancy also causes some breast cells to resist carcinogenic stimuli.[2] So yes, there can be a post-pregnancy bump in estrogen-driven breast cancer, but that cancer already existed.
- It is true that older childbearing women demonstrate a slight increase in breast cancer relative to their never-pregnant peers, but this is for reason #2 above, and is temporary.[3]
- A multitude of studies conclude that prospective moms using any of the ovarian stimulation medications associated with boosting fertility or undergoing IVF, including clomiphene citrate (Clomid), gonadotropin-releasing hormone (GnRH antagonist, Lupron), human chorionic gonadotropin (hCG), follicle stimulating hormone (FSH), luteinizing hormone (LH), and progesterone, do not have a higher risk of breast cancer.[4] In fact, it might be lower.
To summarize: Preston’s later-age pregnancy with baby Ben had no causative relationship to her breast cancer.
Quick Facts About Metastatic Breast Cancer
More than 3.8 million US women with a history of breast cancer are alive today, whether cancer-free or undergoing treatment.[5] Knowing that stage I cancers have a 99 percent 5-year survival rate might create a false sense of cancer curability. The truth is, despite our best efforts, about 25 percent of women initially diagnosed with early-stage breast cancer (that is, not stage IV) eventually develop metastatic disease to a distant organ; but remember, increasingly effective therapies and earlier detection continue to improve this number.[6] Approximately 155,000 women in the United States are alive today with metastatic breast cancer (MBC), which means that cancer cells have metastasized beyond the breast and nearby axillary nodes to other organs or distant nodes, making them stage IV. The most commonly involved areas are lung, liver, brain, and bone. At the time of diagnosis, 6 percent of breast cancers will already have metastasized and be stage IV. While over 11 percent of MBC patients survive more than ten years, the majority (73 percent) will unfortunately live less than five years.[7]